
Welcome to VisionTMS
VisionTMS is an innovative radiologist and psychiatry collaboration specialising in the treatment of mental health disorders, including major depression. We enable your patient to access state-of-the-art TMS treatment at specialist Vision XRAY Group’s practices as an alternative to psychiatry consulting rooms that don’t provide colocated MRI image-guided TMS treatment.
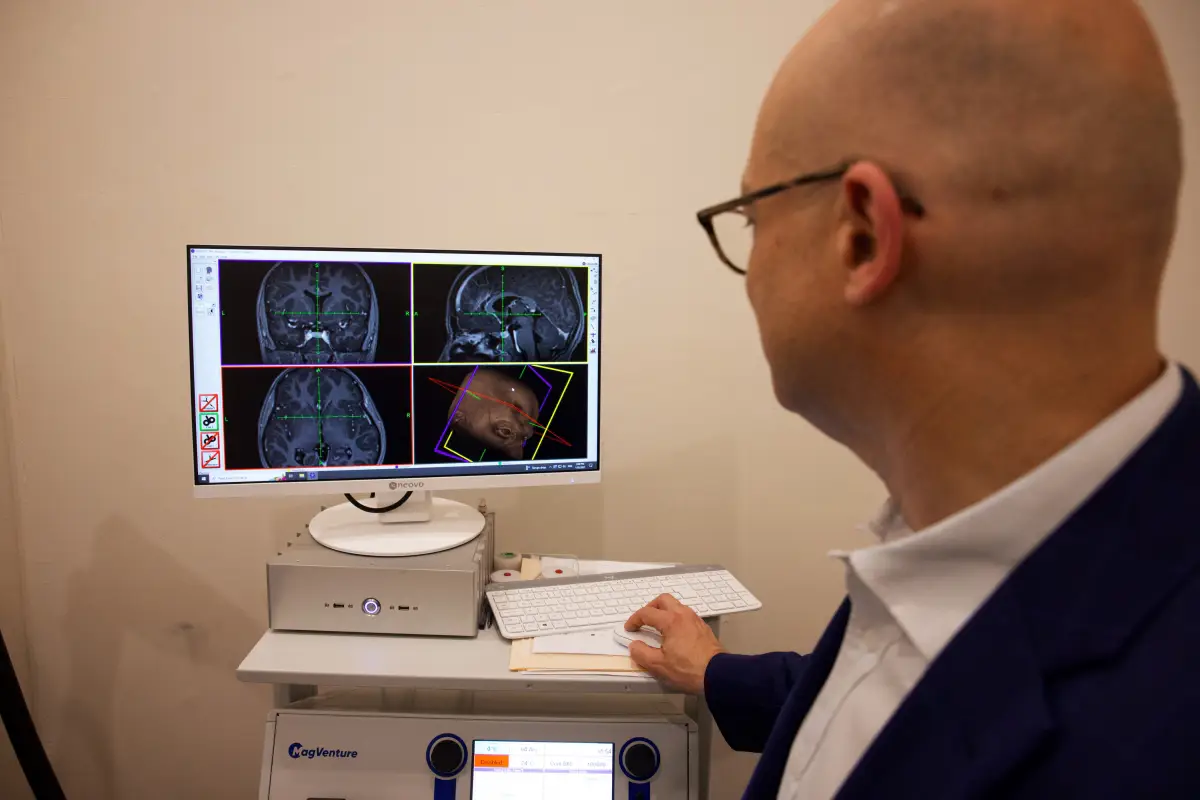
The TMS Image-Guidance Experts
As experts in MRI and image-guided procedures, we specialise in enhancing TMS by using brain MRI to improve treatment precision for the best outcome possible. Our compassionate and patient-centred radiology practices offer the utmost discretion in a supportive clinical environment.


How to refer your patient
Please contact us by:
Does Transcranial Magnetic Stimulation (TMS) really work?
Yes. TMS has been used safely for 30 years and is increasingly recognised as a successful and safe mental health treatment option for patients. Furthermore, there is strong evidence in favour of TMS’s effectiveness in treating Major Depressive Disorder (see the section below). In addition:


How does TMS work?
Evidence for the use of rTMS in depression
rTMS treatment of depression is supported by large-scale real-world outcome data, including:
Please get in touch with our expert team for more information about research, trial and report findings.
THE TREATMENT
How we care for and treat patients
1
As a GP or psychiatrist, you will need to refer your patient to us.
2
Your patient will consult with our TMS Coordinator, who will explain and plan their TMS pathway.
3
Your patient will then undergo MRI mapping to identify the precise brain location for treatment. This tells us where to direct the narrow beam of magnetic energy created by the TMS machine to stimulate the relevant brain cells.
4
This mapping is followed by a dosing session with our TMS-trained consultant psychiatrist. ‘Dosing’ ensures your patient receives the appropriate dose of magnetic energy, as everyone’s optimal dose is slightly different.
5
Your patient then returns to their local Vision XRAY practice for a course of TMS treatments that are precision delivered by our VisionTMS consultant psychiatrist. During treatments, our team continues to guide, support and care for your patient.
6
For more information about the patient sessions, please visit the Patient page.
Process

eLearning to Support Your Patients
VisionTMS is proud to partner with MindSkiller®, an engaging and effective eLearning and eTraining platform that enhances mental health literacy for help providers.
Through MindSkiller®, you can access specialist-grade knowledge, skills and strategies to optimise your patient’s mental health treatment while gaining accredited certification.
MindSkiller® also offers patients an eLearning platform to use alongside their VisionTMS treatments and assist in their journey to good mental health.
EXPLORE MINDSKILLER®Patient Medicare Cover
Initial TMS Treatment Course
Medicare provides cover if your patient meets the following criteria:
TMS Retreatment Course
Medicare provides cover if your patient meets the following criteria:
TMS Booster Course
Medicare does not usually provide cover unless:
Medicare cover FAQs
What is the definition of Major Depressive Disorder (MDD)?
Diagnostic criteria set out in the International Statistical Classification of Diseases and Related Health Problems – 11th Revision (ICD-11) and the Diagnostic and Statistical Manual of the American Psychiatric Association – Fifth Edition (DSM-5) should guide the clinician.
How is a major depressive episode diagnosed for Medicare eligibility?